When are the Medicare enrollment periods?
If you’re about to become Medicare eligible, you need to make some decisions about your health care coverage. This is because if you wait to enroll until after the initial enrollment period, you may have to pay a penalty and there may be a gap in your coverage.
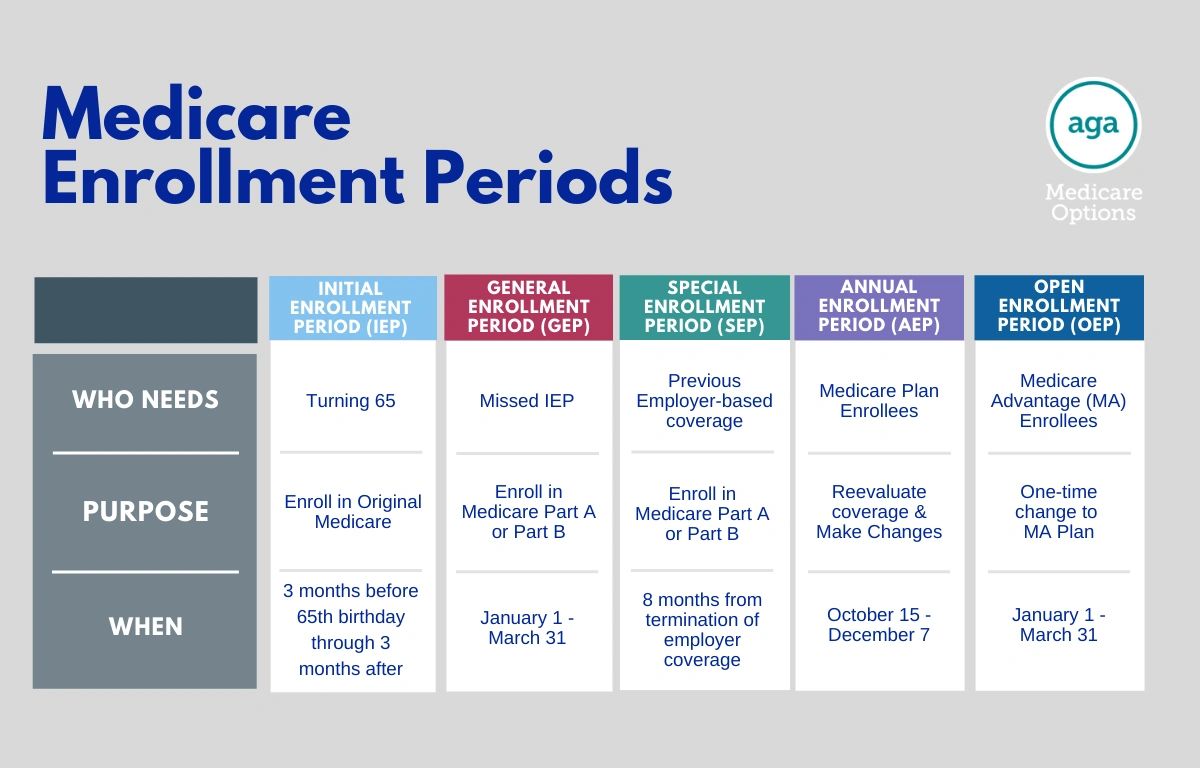
There are five main enrollment periods; Initial Enrollment Period (IEP; for those just turning 65), General Enrollment Period (GEP; for those who did not enroll during IEP), Special Enrollment Period (SEP; for those who had previous health insurance from an employer but now require Medicare Part B), Annual Enrollment Period (AEP; once a year, all individuals on Medicare can re-enroll and change their plans), and Open Enrollment Period (OEP; strictly for those on a Medicare Advantage Plan).
Once you’ve decided what parts of Medicare you would like to enroll in, it’s time to figure out when your plan’s enrollment period is. If you need any assistance in deciding which parts of Medicare to enroll in, give us a call.
Medicare Enrollment Help
If you need help understanding when you enrollment period is and how you can sign up for a policy or plan, give us a call and we can determine your enrollment period for you!
Medicare Enrollment FAQs
Please reach out to us at [email protected] or give us a call if you cannot find an answer to your question.
What if I missed my Medicare Enrollment Period?
If you miss your initial enrollment period, there are a few penalties you’ll face. However, these only apply if you do not have any other coverage, such as employer coverage.
The penalties are as follows:
- If you do not enroll in Part B during initial enrollment, you’ll pay a late enrollment penalty. The penalty is an extra 10% of your premium for every 12-month period you should have had Part B. That 10% is tacked on each month for as long as you have coverage.
- If you don’t have Part D coverage and miss your enrollment period, you’ll pay a late enrollment penalty. The penalty is an extra 1% of your premium for as long as you have coverage.
- Should you not qualify for free Part A coverage because you didn’t work long enough and you miss your enrollment period, you’ll pay an extra 10% of your premium for twice the number of years you didn’t have coverage.
What if I have employer coverage?
Many people work beyond age 65 and would like to continue their employer coverage instead of signing up for Medicare. This is fine and you will not be penalized. When you do retire, you will be able to sign up for Medicare during a Special Enrollment Period.
This enrollment period is eight months long that begins either the month you or your spouse quits working or the month your group coverage ends, whichever comes first.
When is Medigap’s Open Enrollment Period?
Once you are enrolled in Medicare Part A and B, there is a six-month open enrollment period for Medigap (Medicare Supplement) plans. This window begins with your Part B effective date and is a one-time election period.

When is the Medicare Initial Enrollment Period?
Your initial enrollment period begins three months before the month of your 65th birthday and ends three months after your 65th birthday month.
This happens with one exception: if your birthday is on the first of the month. This will cause your enrollment period to begin one month early. For example: if your birthday is October 1, your enrollment period will begin June 1 and your Medicare will begin one month early as well — September 1.
During your initial enrollment period, you can enroll in Original Medicare (Part A and B), Medicare Advantage Plans, or Medicare Part D.
Initial Enrollment Help
Need help determining your Initial Enrollment Period? Find out today!
When is the Annual Enrollment Period?
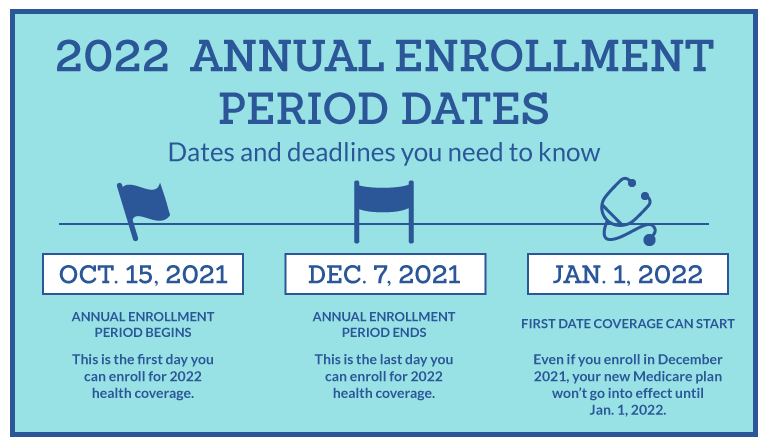
The Medicare Annual Enrollment Period – AEP for short – is a set time each year for changing your Medicare coverage choices if you choose to. AEP runs from October 15 to December 7. New coverage choices go into effect on January 1.
Medicare AEP is a time for you to reevaluate your current coverage and make changes as need be.
The changes you can make during AEP depend on your current coverage. Check you situation below for a run-down on what you can do.
Annual Enrollment Help
Not sure about which plan to choose during Annual Enrollment? Give us a call and we can help to determine which plan best fits your situation!
What changes can I make during AEP?
Please reach out to us at [email protected] or give us a call if you cannot find an answer to your question.
I currently have just Original Medicare (Parts A & B)
- Join a Medicare Advantage plan (Part C) with or without built-in drug coverage. Note that you may be charged a penalty if you do not currently have other creditable drug coverage.
- Join a stand-alone Medicare prescription drug plan (Part D). A penalty may apply here as well if you do not currently have other creditable drug coverage.
- Make no changes and your current coverage will renew as is.
I currently have Original Medicare (Part A and/or B) and a stand-alone Medicare Prescription Drug Plan (Part D)
- Join a Medicare Advantage plan (Part C) with or without built-in drug coverage.
- Switch from your current Medicare prescription drug plan to another Medicare prescription drug plan.
- Drop Medicare prescription drug coverage completely. Note that you may be charged a penalty if you decide you want drug coverage again later.
- Make no changes and your current coverage will renew as is.
I currently have a Medicare Advantage plan (Part C) with built-in drug coverage
- Switch from your current Medicare Advantage plan to another Medicare Advantage plan with or without built-in drug coverage.
- Drop your Medicare Advantage plan and go back to Original Medicare.
- Join a stand-alone Medicare prescription drug plan if you go back to Original Medicare or if you switch to a Medicare Advantage plan that does not include drug coverage.
- Drop Medicare prescription drug coverage completely. Note that you may be charged a penalty if you decide you want drug coverage again later.
- Make no changes and your current coverage will renew as is.
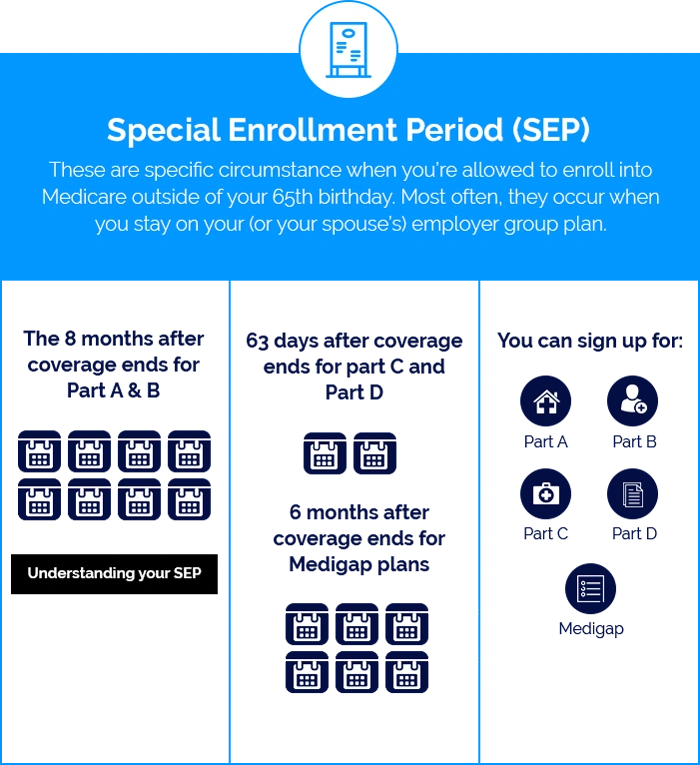
What is a Medicare Special Enrollment Period?
There are a couple situations that allow you to enroll into Medicare during a Special Enrollment Period.
As discussed above, if you work beyond age 65 and have employer-provided health coverage that you would like to continue instead of Medicare, you are allowed to delay enrollment without penalty.
Another example would be if you move outside of a plan’s service area. This would trigger a two-month enrollment period in which you could switch to a new Medicare Advantage or Part D prescription drug plan. You could also return to Original Medicare without penalty. Sometimes, you can also enroll into Medigap.
There are other unique situations in which you may also be eligible for a special enrollment period. You are welcome to contact us to learn what options are available for you.
Special Enrollment Help
Need help determining if you qualify for a special enrollment period? Give us a call today and we can determine for you!
